Prostate pathology outlines
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience!
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience! Page views in 7, Cite this page: Sanguedolce F. Nonspecific granulomatous prostatitis.
Prostate pathology outlines
This review article focuses on prostate carcinoma and underscores changes in the prostate chapter as well as those made across the entire series of the 5th edition of WHO Blue Books. Evolving and unsettled issues related to grading of intraductal carcinoma of the prostate and reporting of tertiary Gleason pattern, the definition and prognostic significance of cribriform growth pattern, and molecular pathology of prostate cancer will also be covered in this review. The publication of WHO Classification of Urinary and Male Genital Tumors 5th Edition marks another major milestone in the field of genitourinary GU pathology and is the culmination of scientific advancements in recent years built upon the 4th edition published in The new edition of this authoritative reference book provides a comprehensive update on tumor classification in the same modular fashion as the previous edition with the addition of several new sections for each disease entity, including cytology, diagnostic molecular pathology, essential and desirable diagnostic criteria, and staging. This review article highlights salient changes made to the prostate chapter as we have gained better understanding of the etiology, pathogenesis, and molecular pathology of prostate cancer. The following topics will be presented in detail: 1 changes in nomenclature and terminology, 2 prostatic ductal adenocarcinoma and prostatic intraepithelial neoplasia PIN -like adenocarcinoma, 3 intraductal proliferative lesions and reporting recommendations from the two major urological societies regarding intraductal carcinoma of the prostate, 4 cribriform growth pattern, 5 reporting of tertiary Gleason pattern, 6 treatment-related neuroendocrine prostatic carcinoma, and 7 molecular genetics. In addition to the updates specific to this chapter, the format of the contents had also been restructured across all volumes of the 5th edition series and that pertaining to the prostate chapter will be addressed first to provide an overview of how the new WHO Blue Book is organized. In alignment with the new format in the 5th edition series, less common but identical neoplasms from various sites in the GU system, i. However, stromal tumors of the prostate, thought to originate from prostate stromal cell proper, and treatment-related neuroendocrine prostatic carcinoma, are still included in the prostate chapter due to their uniqueness to the prostate, and distinctive biological and clinical characteristics as well as therapeutic implication for the latter. Likewise, urothelial carcinoma of the prostate and prostatic urethra, is now incorporated into Chapter 3, Tumors of the Urinary Tract, for similar reasons, while maintaining the pT staging criteria for pT2 transmucosal invasion of the prostatic stroma and pT4 transmural or extravesical invasion from the urinary bladder into the prostatic stroma from the previous edition. With more than half of the tumors discussed in other chapters, only 11 tumor types remain in the prostate chapter Tab. These tumors are divided into two broad categories: epithelial tumors and mesenchymal tumors unique to the prostate. The epithelial tumor category is further subcategorized into two families: glandular and squamous neoplasms. The glandular family comprises 6 tumor types: cystadenoma, high-grade prostatic intraepithelial neoplasia HGPIN , intraductal carcinoma of the prostate IDC-P , prostatic acinar adenocarcinoma acinar PCa , prostatic ductal adenocarcinoma ductal PCa , and treatment-related neuroendocrine prostatic carcinoma t-NEPC. The squamous family comprises 3 tumor types: adenosquamous carcinoma, squamous cell carcinoma, and adenoid cystic basal cell carcinoma of the prostate.
Eur Urol ; 68 Figure 6.
Maintenance between March 11 and 12 may cause some brief downtime. We apologize for any inconvenience! Page views in 6, Prostate specific antigen PSA. Accessed March 11th, Androgen regulated serine protease Encoded by kallikrein gene KLK3 , kallikrein related peptidase 3 located on chromosome 19 Endocr Rev ; Essential features.
We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:. Biopsy and Cytology Tests. Biopsy samples collected from your prostate are studied by a doctor with special training, called a pathologist. After testing the samples, the pathologist creates a report on what was found. Your doctor can use this report to help manage your care.
Prostate pathology outlines
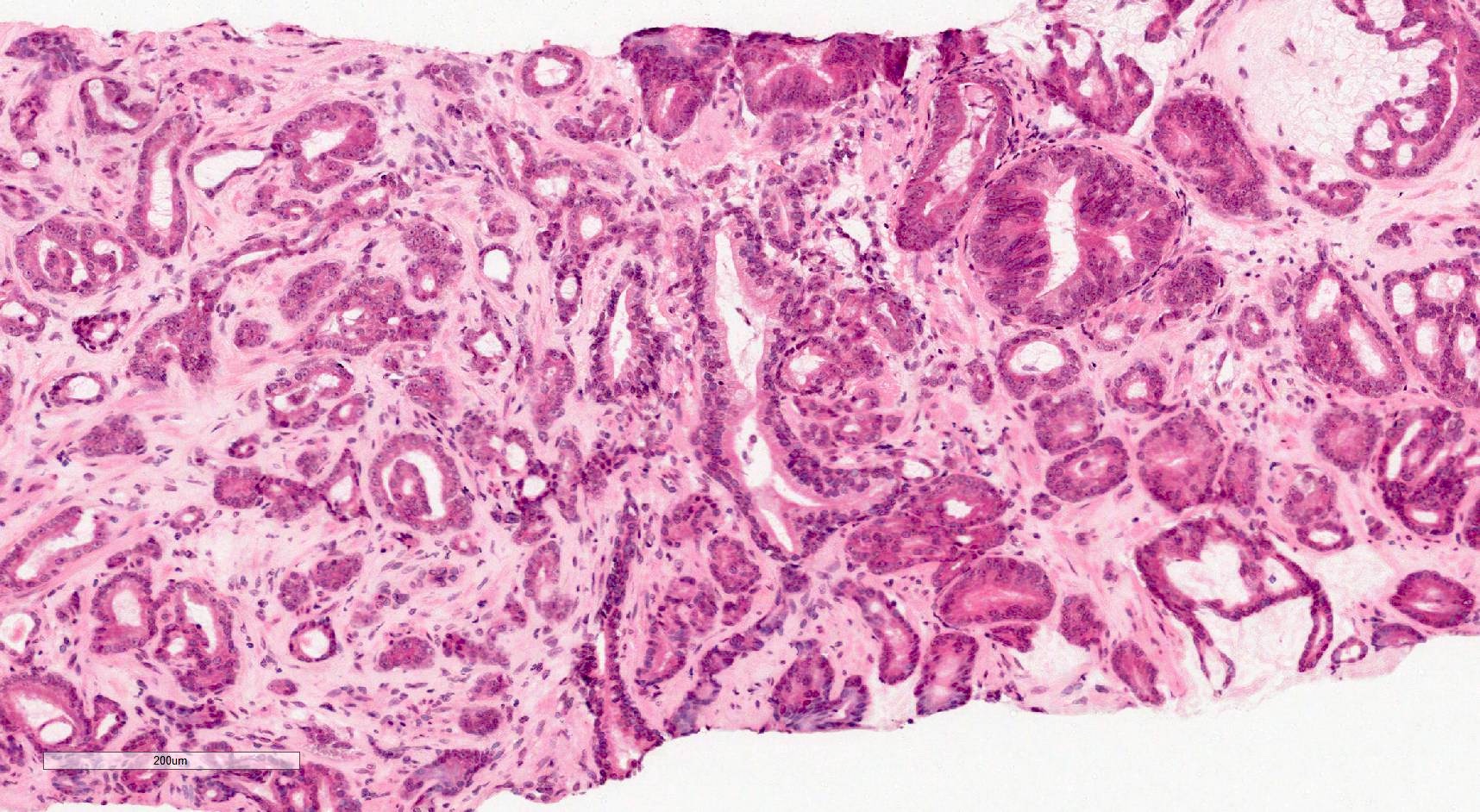
Four major pathologic entities will be discussed in this topic review: prostatic intraepithelial neoplasia PIN , atypical adenomatous hyperplasia AAH, also termed adenosis , atrophic lesions, and atypical small acinar proliferation ASAP. High-grade PIN is the most likely precursor of the majority of prostatic adenocarcinomas. In contrast, AAH and atrophic lesions are possible, although uncertain, precancerous lesions. ASAP is not a true biologic entity but is a diagnostic term in pathology when a lesion suspicious for but not diagnostic of carcinoma is identified. The pathologic characteristics, prevalence, relationship to prostate cancer, and clinical significance of these lesions are discussed in this topic, with a particular emphasis on PIN. Histology — The histologic characteristics of PIN have been well described [ 5,6 ]. The neoplastic prostatic epithelial cells are within prostatic ducts or acini, which are typically large and branched, with a convoluted inner contour similar to benign glands picture 1. Epithelial cell proliferation produces a layer of crowded, pseudostratified, neoplastic cells with cytologic atypia, characterized by nuclear irregularity, nucleomegaly, hyperchromasia, and prominent nucleoli picture 1.
Kissing with sexy
Treatment-related neuroendocrine prostatic carcinoma t-NEPC. In fact, ductal PCa comprises 2. Consequently, this lesion is no longer diagnosed in the WHO Blue Book and should not be reported for several reasons, including poor reproducibility and no increased risk of cancer detection in subsequent biopsies Due to mounting molecular evidence, there have been discussions to reclassify ductal PCa as a subtype of acinar PCa rather than retaining it as a separate tumor type 2. Accessed March 11th, This recommendation from GUPS, therefore, is not a modification of the grading rules but rather a clarification of the conventional grading rules currently in use. Mod Pathol ; 31 S1 :S Zynger, M. The new edition of WHO Blue Book acknowledges these dissimilarities but does not endorse either position because the overall evidence is insufficient, and both positions are mainly based on consensus opinions However, we cannot answer medical or research questions or give advice. Click here for information on linking to our website or using our content or images. Accessed March 11th,
Check out our latest pathology themed Wordle here! Updated every Monday. Page views in ,
CCR Prostatic acinar adenocarcinoma. Board review style question 2. Usually located in posterolateral soft tissue outside of prostate Seen in radical prostatectomy specimens and rarely in prostate needle biopsies, or in smooth muscle of bladder neck in transurethral resections of prostate or bladder. In fact, ductal PCa comprises 2. Figure 3. There should be no intervening stroma or mucin separating individual or fused glandular structures. Other more subtle changes are the standardization of mitotic counts, genomic nomenclatures, and units of length. This inevitably led to another discordant views regarding the use of basal cell markers to differentiate IDC-P from invasive PCa. Controversial issues related to discordant recommendations from GUPS and ISUP have been acknowledged and will likely be revisited in the next edition when more solid evidences are available.

What talented idea