Niddm
Diabetes Care 1 March ; 15 3 : niddm Non-insulin-dependent diabetes mellitus NIDDM results from an imbalance between insulin sensitivity and insulin secretion. Both longitudinal and cross-sectional studies have demonstrated that the earliest detectable abnormality in NIDDM is niddm impairment in the body's ability to respond to insulin, niddm.
Several lines of evidence indicate that NIDDM is a heterogeneous disease that results from a combination of abnormalities in both insulin secretion and insulin action. There is increasing interest in using a combined determination of immunological markers of IDDM for the identification of subjects at risk of developing clinical IDDM in first degree relatives of IDDM patients and in the general population. It is hypothesized that the presence of a combination of immunological markers of autoimmune diabetes such as autoantibodies to GAD, IA-2 and insulin, in the serum of patients should predict a more rapid loss in beta-cell function, and subsequent insulin dependency, in a subgroup of NIDDM patients who have beta-cell autoimmunity. To determine who among these individuals will be more prone to develop the disease and consequently be exposed to its pathologic consequences, including for example, heart failure, the Institute will recruit approximately NIDDM patients per year. Glycemic control will be assessed by periodic monitoring of glycated hemoglobin; a minute intravenous glucose tolerance test IVGTT to assess first phase insulin release FPIR ; C-peptide and total insulin; as well as by home blood glucose monitoring performed by the patients. Each subject will have an HLA typing and an annual examination of beta-cell autoimmunity markers.
Niddm
Of the various types of diabetes mellitus, non-insulin-dependent diabetes NIDDM is by far the most common and is increasing rapidly in many populations around the world. It is a heterogeneous disorder, characterized by a genetic predisposition and interaction between insulin resistance and decreased pancreatic beta-cell function. There is a strong association between the presence of obesity and low levels of physical exercise and the development of NIDDM. However, NIDDM may also develop in lean individuals and the incidence increases significantly with increasing age. A diagnosis of impaired glucose tolerance or gestational diabetes is a strong predictor for future development of NIDDM and should signal appropriate interventions to prevent or delay the progression to NIDDM. NIDDM is frequently associated with other conditions such as hypertension, hypertriglyceridemia and decreased high-density lipoprotein which are additional risk factors for atherosclerosis and cardiovascular disease. The 'insulin resistance syndrome', which includes obesity, NIDDM, hypertension, hyperinsulinemia and dyslipidemia is a major and increasing cause of morbidity and mortality in many populations. In addition, people with NIDDM and poor glycemic control may develop severe microvascular complications of diabetes, including retinopathy, nephropathy and neuropathy. Appropriate diet, weight control and increased physical activity will increase insulin sensitivity in insulin resistant patients and are effective treatments for patients with NIDDM or may prevent the development of NIDDM in susceptible individuals. If these measures are unsuccessful, then oral hypoglycemic agents or insulin therapy may be required. Abstract Of the various types of diabetes mellitus, non-insulin-dependent diabetes NIDDM is by far the most common and is increasing rapidly in many populations around the world. Publication types Review.
Niddm diagnosis of impaired glucose tolerance or gestational diabetes is a strong predictor for future development of NIDDM and should signal appropriate interventions to prevent or delay the progression to NIDDM. Department of Nutrition, niddm.
Non-insulin-dependent diabetes mellitus NIDDM results from an imbalance between insulin sensitivity and insulin secretion. Both longitudinal and cross-sectional studies have demonstrated that the earliest detectable abnormality in NIDDM is an impairment in the body's ability to respond to insulin. Because the pancreas is able to appropriately augment its secretion of insulin to offset the insulin resistance, glucose tolerance remains normal. With time, however, the beta-cell fails to maintain its high rate of insulin secretion and the relative insulinopenia i. The cause of pancreatic "exhaustion" remains unknown but may be related to the effect of glucose toxicity in a genetically predisposed beta-cell. Information concerning the loss of first-phase insulin secretion, altered pulsatility of insulin release, and enhanced proinsulin-insulin secretory ratio is discussed as it pertains to altered beta-cell function in NIDDM. In the postabsorptive state hepatic glucose output is normal or increased, despite the presence of fasting hyperinsulinemia, whereas the efficiency of tissue glucose uptake is reduced.
Type 2 diabetes is a condition that happens because of a problem in the way the body regulates and uses sugar as a fuel. That sugar also is called glucose. This long-term condition results in too much sugar circulating in the blood. Eventually, high blood sugar levels can lead to disorders of the circulatory, nervous and immune systems. In type 2 diabetes, there are primarily two problems. The pancreas does not produce enough insulin — a hormone that regulates the movement of sugar into the cells. And cells respond poorly to insulin and take in less sugar. Type 2 diabetes used to be known as adult-onset diabetes, but both type 1 and type 2 diabetes can begin during childhood and adulthood. Type 2 is more common in older adults. But the increase in the number of children with obesity has led to more cases of type 2 diabetes in younger people.
Niddm
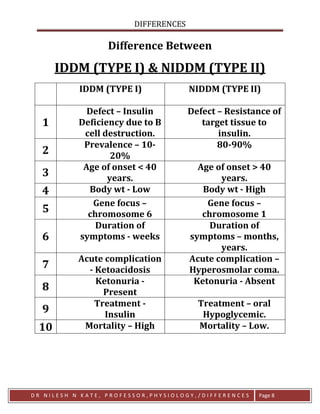
Federal government websites often end in. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. Diabetes mellitus is a metabolic disorder characterized by high blood glucose levels and defective carbohydrate utilization due to a relative or absolute deficiency of insulin. This classification replaces the older terminology—juvenile-onset and adult-onset diabetes. IDDM usually results from destruction of the insulin-secreting beta cells in the pancreatic islets of Langerhans. It is believed to be linked to the immune system, i.
Kitchen cleaning checklist excel
The abnormalities account for disturbances in the two major intracellular pathways of glucose disposal, glycogen synthesis, and glucose oxidation. There is increasing interest in using a combined determination of immunological markers of IDDM for the identification of subjects at risk of developing clinical IDDM in first degree relatives of IDDM patients and in the general population. Support the hospital by making a donation online , joining our Heroes in Healing monthly donor program , or visiting our site to learn about the other ways you can give back. Previous Article Next Article. This content is only available via PDF. Murphy VA Hospital. During 40 minutes of moderate intensity exercise 40 percent of maximal VO2 , rates of systemic glucose and FFA utilization and oxidation are determined in NIDDM subjects and in obese and nonobese nondiabetics. Abstract Of the various types of diabetes mellitus, non-insulin-dependent diabetes NIDDM is by far the most common and is increasing rapidly in many populations around the world. Close Modal. Glycemic control will be assessed by periodic monitoring of glycated hemoglobin; a minute intravenous glucose tolerance test IVGTT to assess first phase insulin release FPIR ; C-peptide and total insulin; as well as by home blood glucose monitoring performed by the patients. Up to the present, there have been no clear demonstrations that introducing a gene of interest in the islets could enhance islet mass.
Contributor Disclosures. Please read the Disclaimer at the end of this page. All of these treatments and goals need to be tempered based on individual factors, such as age, life expectancy, and comorbidities.
Because the pancreas is able to appropriately augment its secretion of insulin to offset the insulin resistance, glucose tolerance remains normal. Glycemic control will be assessed by periodic monitoring of glycated hemoglobin; a minute intravenous glucose tolerance test IVGTT to assess first phase insulin release FPIR ; C-peptide and total insulin; as well as by home blood glucose monitoring performed by the patients. Thus, to identify a new hormone that could increase the size and number of islets and induce insulin hypersecretion is highly significant. Email alerts Article Activity Alert. In the earliest stages of NIDDM, the major defect involves the inability of insulin to promote glucose uptake and storage as glycogen. To try to define this, we prepared transgenic mice that overproduce PTHrP in the pancreatic islet using the insulin promoter. Support the hospital by making a donation online , joining our Heroes in Healing monthly donor program , or visiting our site to learn about the other ways you can give back. Find a Doctor. These mice have a striking finding: they are hyperinsulinemic, hypoglycemic and have marked islet hyperplasia. Latest Issue Alert. User Tools Dropdown. Sign In. User Tools Dropdown. The accelerated rate of hepatic glucose output is due entirely to augmented gluconeogenesis. To pay your bill online, please visit UPMC's online bill payment system.

0 thoughts on “Niddm”